Body
The Journal of Neurophysiology recently published a review by Adenike Adewuyi, MD PhD — a 2022 graduate of Shirley Ryan AbilityLab’s physical medicine and rehabilitation (PM&R) residency program — and her mentor, Colin Franz, MD, PhD, physician-scientist, at Shirley Ryan AbilityLab. The review defines a clinical framework for evaluating patients with spinal cord injuries to determine their candidacy for nerve transfer surgery.
In a patient with spinal cord injury, Dr. Adewuyi said, there is damage to the nerve that otherwise brings information from the brain to the spinal cord. “With nerve transfer surgery, the idea is to bypass that block — that damage — by going above that injury, to ‘rewire’ it and reconnect it above the injury,” she said. “But, if you’re going to ‘rewire’ the nerve, you need to make sure that the wire you're using is intact and working normally.”
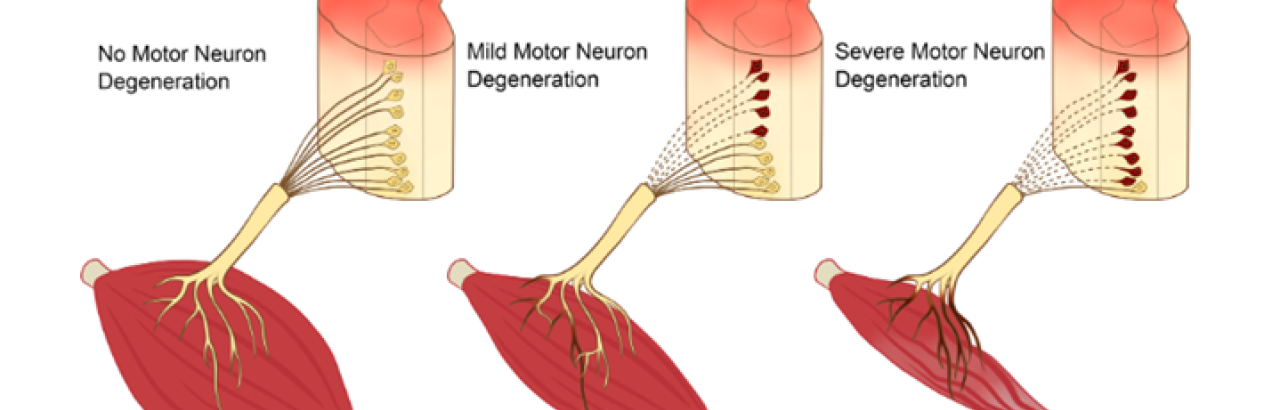
“We can't take for granted that the connections to the muscles are always intact,” Dr. Franz said. “For some patients that is true; but, for others, some nerve-muscle connections are compromised. For them, we need to use different approaches, like tendon transfer, to restore the arm function.”
To ensure that nerve transfer surgery will benefit patients, the Journal of Neurophysiology review proposes evaluation protocols by electrodiagnostic clinicians to determine the health and ability of motoneurons to communicate between the spinal cord and muscles. It also includes post-operative rehabilitation plans. “Our proposed evaluation protocol can have implications for the potential surgeries for which patients are candidates,” Dr. Adewuyi said.
IMPACT: “This approach is personalized medicine for restoring arm function after spinal cord injury,” Dr. Franz said. “We want to make sure that we get the best outcome for patients, whether that’s using reconstructive tendon surgery versus nerve transfer surgery, or even making the decision to intervene earlier if that’s needed.” Dr. Adewuyi is now a neuromuscular fellow at Northwestern University Feinberg School of Medicine’s Department of Neurology. She conducted research for this review — for which she recently received the Foundation for PM&R’s New Investigator Award — while she was in residency at Shirley Ryan AbilityLab.