Body
A new study published in the October 2022 issue of the Journal of NeuroEngineering and Rehabilitation from a research team led by SRAlab clinicians identified the cause of — and hope for a potential prevention of — nerve injuries in patients treated in the intensive care unit for severe COVID-19.
The study’s lead author, Colin Franz, MD, PhD, physician-scientist, said the research identified two novel findings: first, it implicated both “mechanical loads” (stress caused compression and stretching) and COVID-19 as the cause of the nerve injuries; and second, it identified the possibility of using wireless sensors to detect and prevent similar injuries among patients in the ICU. This study was supported by a generous philanthropic gift from the family of Belle Carnell, which established a regenerative neurorehabilitation fund to overcome barriers that impede timely, innovative research to address clinical challenges that arise in the COVID pandemic and beyond.
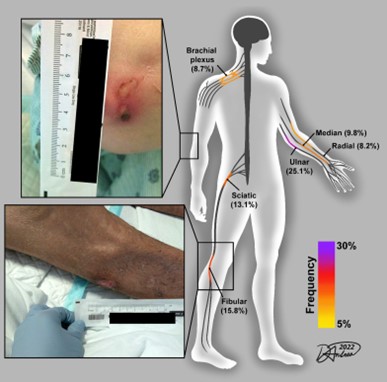
The team’s innovative research built on a 2020 quality improvement study by Dr. Franz and his collaborators that identified surprisingly high rates of nerve injuries in patients in the ICU with severe COVID-19. This study identified nerve injury “hot spots”: the 6 out of 20 locations on the body that accounted for more than 80% of all nerve injuries in patients with severe COVID-19. With this data, they provided best practices for positioning to prevent those nerve injuries from occurring in places like knees and elbows.
After further research by other teams confirmed a link between COVID-19 and nerve damage, Dr. Franz and his collaborators sought to expand their scope.
“Our follow-up study — a multicenter effort between researchers at SRAlab, Marionjoy and Northwestern Memorial — is the largest single study of its kind. We looked at 34 new cases and re-analyzed another 58 patients from published case reports,” he said.
Their findings show that both severe COVID-19 infection and ICU treatments and positioning are the main factors behind these nerve injuries.
“Based on the locations and clinical patterns we discovered, we concluded that most of the nerve injuries occurred from mechanical loads in these patients who were unusually susceptible to nerve damage,” said Dr. Franz. “They were about 10 times more likely to occur in these patients with severe COVID than in non-COVID inpatient rehabilitation patients.”
IMPACT: Dr. Franz said the new research also provides “proof on concept” for the use of wireless sensors for real-time monitoring of patients to prevent nerve injuries from even occurring. “The answer to ‘when’ that will happen depends more on industry partnership and healthcare policy then on our preclinical science,” he said. “For example, we track pressure injuries to skin acquired in hospitals so there’s a lot of clinical effort and technology deployed to prevent them. However, mechanical nerve injuries are not well monitored or tabulated as a matter of routine clinical care, so the first step to implementation of this technology is for healthcare systems and policy makers to appreciate the issue.”