Body
Cassandra H., 63, has spent a lifetime on her feet. She was a clinical pharmacist and worked on her feet most days while helping patients. As a young woman, she played volleyball, basketball and ran track. She has continued to enjoy physical activities like bowling, golfing and exercising.
About six years ago, Cassandra was slowed down after breaking her left foot. She had an “unremarkable recovery” in which she wore a boot for six weeks as her foot healed … but then, one day at work, she noticed her foot was still hurting. As it turned out, she had fractured sesamoid bones — the bones located under the big toe joint — and foot surgery was required.
From there, complications continued for several years. Cassandra ultimately needed to have a more involved procedure — reconstructive foot surgery. She had long periods of immobilization, and her ongoing foot issues took her away from her job.
With two surgeries behind her, Cassandra just wanted to get back to the life she loved. Unfortunately, she started experiencing excruciating nerve pain in her left foot and needed to use a wheelchair because she no longer could bear weight on it.
“My pain journey has been long,” said Cassandra. “I would have electric shock-type pain. My foot would swell to five times its size and change colors from red to purple. I couldn’t tolerate anything touching it. The water in the shower caused unbearable pain, and I couldn’t even wear a sock because it was so painful.”
Finally, five months after the reconstructive foot surgery, Cassandra was diagnosed with complex regional pain syndrome (CRPS), a chronic pain condition that can occur in patients who have had trauma to a certain part of their body from surgery, immobilization or other injury.
While therapy, injections and medication usually are prescribed for the treatment of CRPS, Cassandra’s pain was extreme. She wanted to find a resource with the expertise she needed … and she discovered the Pain Management Center at Shirley Ryan AbilityLab.
Interdisciplinary Treatment for Chronic Pain
Body
The Pain Management Center is one of the only interdisciplinary pain clinics in the country that offers a novel, team-based approach in which medical doctors, psychologists, physical therapists and occupational therapists collaborate to help patients with pain.
With an active-care environment, Shirley Ryan AbilityLab’s clinicians provide a path to relief by offering patients skilled treatment, education, and tools and strategies to better manage their pain.
Patients typically participate in a 4-6 week outpatient program, attending individual therapy and group sessions anywhere from 3-35 hours per week (depending on the severity and complexity of their condition and as determined by Shirley Ryan AbilityLab’s team evaluation).
When Cassandra came to the Pain Management Center for the first time, she met with Karina Bouffard, MD, MPH, an attending physician at Shirley Ryan AbilityLab who specializes in treating subacute and chronic pain.
Dr. Bouffard recommended that Cassandra receive a spinal nerve block, an injection to treat pain, before starting the program and in order to more easily tolerate the therapeutic interventions.
“I was still in a wheelchair because my pain was as bad as it had ever been, but Dr. Bouffard assured me I could start the program when I was ready,” said Cassandra.
When she was ready, she got right to work.
Retraining the Brain About Pain
Body
An important part of learning how to manage chronic pain is retraining the brain through a series of small steps that increase in difficulty. This helps patients learn how to tolerate and eventually participate in activities, while better managing their pain.
“I learned that my brain was trying to protect my foot through pain, but I actually needed to reprogram it to start reducing my pain,” said Cassandra.
In physical therapy, she worked on an anti-gravity treadmill which uses air pressure technology to reduce gravitational forces and “lift” a person off the treadmill, enabling her to start bearing weight again.

Meanwhile, Cassandra also participated in mirror therapy during physical and occupational therapy. While Cassandra’s pain was in her left foot, in mirror therapy, she would look at her right foot — her “good foot”— in the mirror. This tricked her brain into believing that the reflection of the right foot was her left, painful foot — an illusion that creates new, positive associations with touch and movement.
“At first, they would touch a Q-tip to my good foot while I was looking at it in the mirror, and even that would hurt,” said Cassandra. “However, over time you trick your brain into thinking you’re looking at the other foot, and you visualize moving it without pain.”
In addition to mirror therapy, aquatic therapy was another way Cassandra slowly built tolerance to touch and move her foot — and reduced her anxiety around pain.
“It took three people to help get me in the pool at first. Even dipping my toe in the water would hurt, but I worked up to being in the pool comfortably and walking around like everyone else,” she said.
Cassandra had two additional lumbar sympathetic blocks during the program, an outpatient injection procedure in the lower back that blocks pain signals to the lower limbs. These blocks provided increasing relief during the program; over time, Cassandra was able to taper off one of her medications without a loss of function nor an increase in pain.
“The Place to Be & The Place for Me”
Body
For eight weeks, Cassandra participated in intensive physical and occupational therapy, met with pain psychologists, attended group sessions with a cohort of other patients living with chronic pain, and educated herself about pain science.
“In only three weeks, they had me up and moving out of a wheelchair,” said Cassandra. “The multidisciplinary approach was completely necessary for me. The spinal blocks helped. I had different types of therapy scheduled every hour. They gave me techniques to work on at home. I even read the book they gave me three times!”
For the first time in a long time, Cassandra’s pain started to recede.
“One day in physical therapy, I was doing my exercises, and my therapist asked me about my pain level,” said Cassandra. “I had zero pain on a scale of one to 10. Beforehand, even when I was on a maximum dose of pain medications, I would have said my pain level was 25. I couldn’t believe it.
“I could tell this was the place to be, and I could tell this was the place for me,” she continued. “Their approach, knowledge base and willingness to help me — everyone really cared for me.”
“Look at That Gait”: Cassandra Celebrates Grad Day
Body
One of Cassandra’s goals at the Pain Management Center was to resume walking unassisted, especially after spending time using a wheelchair during her worst moments of pain.
“I told everyone, ‘I’m not leaving until I walk out of here,’” she said — and she met that goal.
On one of her final days at Shirley Ryan AbilityLab, Cassandra’s care team captured her on video walking on her own, saying “heel toe, heel toe, look at that gait!” as her therapists cheered her on. In another video, she’s doing jumping jacks.
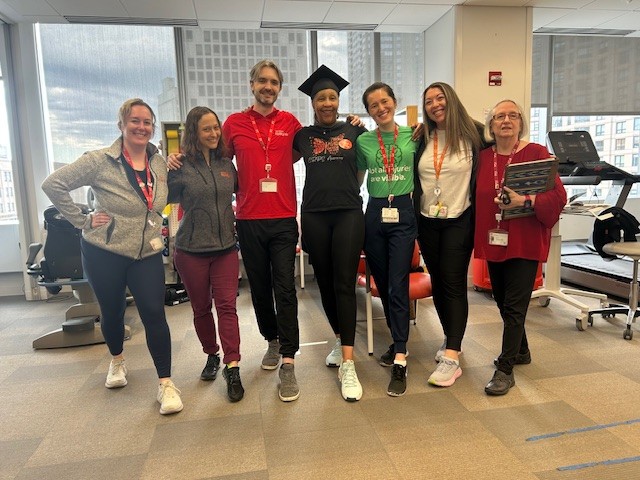
On her “grad day” from Shirley Ryan AbilityLab, she wore her actual graduation cap from pharmacy school and celebrated with her therapy team. She also wore a “CRPS Awareness” T-shirt as a nod to her journey.
Cassandra continued outpatient physical therapy at Shirley Ryan AbilityLab for a few additional months and, today, she is equipped with new skills and techniques for managing pain, such as using pacing strategies to know when to take breaks from activity.
Now retired, she is getting back to recreational activities she enjoys without using a wheelchair or crutches. She also celebrates small things others take for granted, like being able to apply nail polish to both feet without experiencing pain.

Occasionally, especially on rainy days, she says her left foot still “talks” to her, but she now is able to manage any flare-ups.
“The black cloud of pain looming over me is gone,” she said. “This program has given me life back, plus some!”

